Module Content
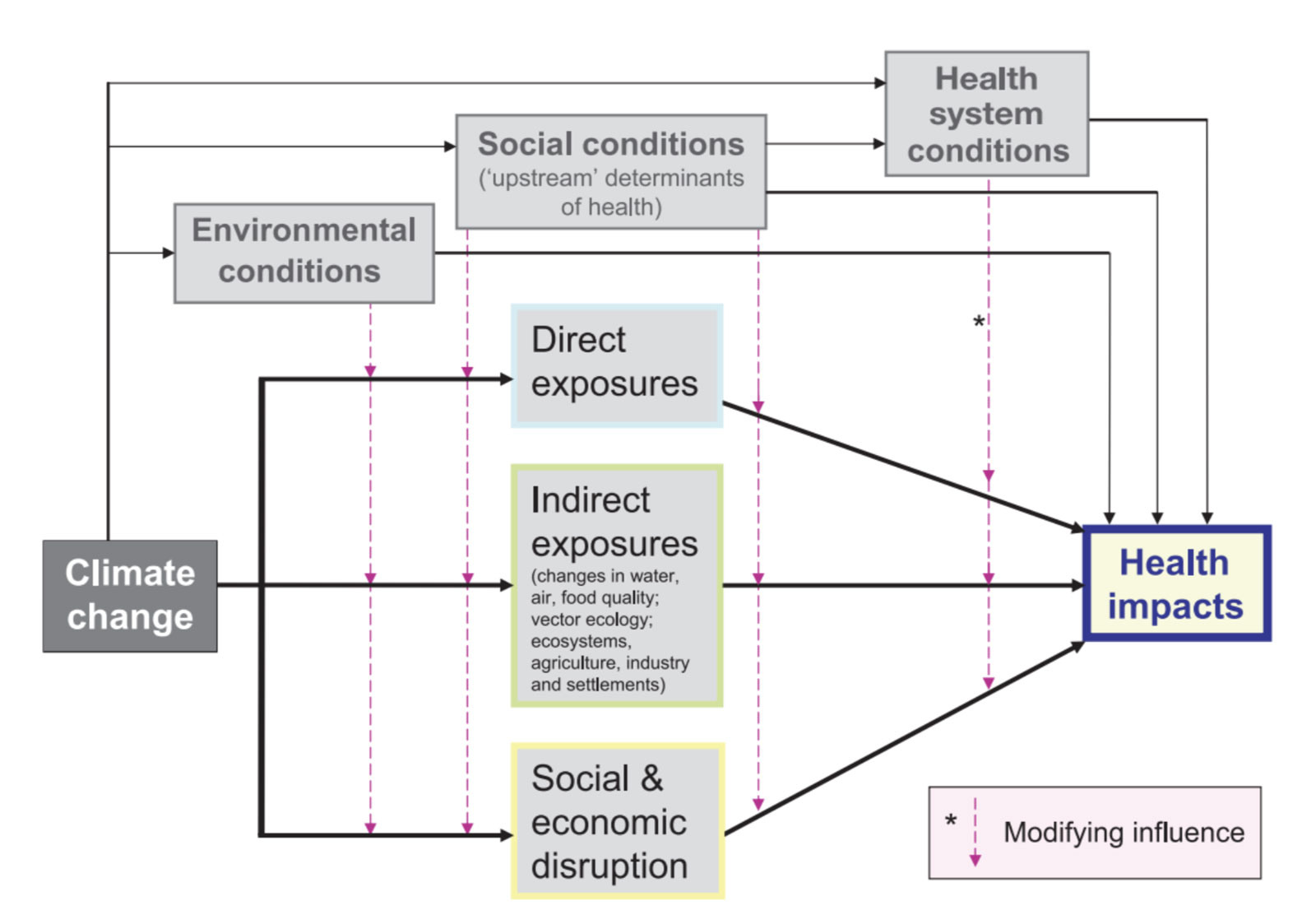
This Health module has been designed and developed to provide information about the priority issues for this sector associated with climate change. After engaging with health professionals and practitioners across Canada both through a survey and focus groups, relevant climate indices and case studies were identified, as well as the best ways of presenting climate information, both visually and for download purposes.
Extreme events, particularly extreme heat, were identified as having the most significant impacts on the health of Canadians. In response to this, a number of heat-related climate indices are available on ClimateData.ca, as well as a case study describing the impact of heatwaves in the province of Quebec. Users can explore how the number of days with maximum temperatures above a variety of temperature thresholds may change in the future in response to low, moderated and high increases in greenhouse gas emissions, and similarly for tropical nights (when minimum temperatures do not fall below specified temperature thresholds). Recognizing that Canada’s vastness means that it is not reasonable to try and define a single heatwave index which has relevance across the country, a number of heatwave indices may be calculated on the Analyze page using custom temperature threshold values.
Another growing public health concern is the increasing incidence of Lyme disease, and the potential for its further spread across Canada as the climate warms. The survival of the black-legged tick, the main vector of Lyme disease, is partially dependent on temperature (annual accumulation in excess of 2800 degree days above 0°C) and, as the climate warms, its range is projected to increase10. ClimateData.ca provides this accumulated degree day index and thus allows users to determine how this tick’s range may change in the future. The accompanying case study for Ontario also details possible adaptation actions to reduce exposure to ticks.
Both extreme heat and Lyme disease are also explored in a case study summarising a report from the Conservation Council of New Brunswick11 on the effects of climate change on the physical and mental wellbeing of people in 16 communities in that province. The impacts of drought on human health and well-being across the southern Prairies and in the interior of British Columbia, are also described in a case study focused on these regions.
Climate change impacts not only the health of Canadians, but also health systems, the hospitals and other infrastructure required to deliver health services to people. These systems are also vulnerable to climate change, not only through extreme events, such as floods, heatwaves and wild fires, which directly impact their operations, but also via the gradual change in climate over time. This will impact the efficiency of, for example, HVAC systems, which may more frequently experience conditions outside of their operating design range. In order to continue to deliver health services efficiently, health systems will need to become increasingly resilient to climate change. Relevant climate indices and options to increase building resiliency in the face of climate change are explored in a case study using examples from British Columbia12,13.